Anatomy
Every person looks different. Our hands, noses and eyes all differ from person to person – and the same goes for vulvas. On this page you’ll find all kinds of information about the vulvar anatomy, accompanied by illustrations.
Take a closer look
Do you know what your vulva looks like? An easy way to find out is to take a look using a hand mirror. Not only can it be very enlightening to see it and get to know all its parts, but knowing your vulva is also very useful as you’ll be able to observe possible changes throughout your life. You can explore your vulva with your eyes and fingers to get to know its shape, and even smell your own scent. This way you will be aware if anything changes: sudden skin discolouration or moles, lumps or a change in the smell or structure of your discharge. By noticing such changes, you’ll be able to get a timely check at your medical health provider if anything seems off.
When opening a textbook about anatomy, you may find that your vulva looks different from the vulvas depicted there. Each and every vulva is unique, so it would be impossible to represent all shapes and sizes in one book. In the following pages, you’ll find a variety of vulva shapes and skin tones – one of these might even resemble your own anatomy.
In my book, A Celebration of Vulva Diversity, I'm showing a variety of vulvas seen from below – in addition to the frontal perspective I usually paint in the gallery. I feel that anatomical diversity should be a fundamental part of any book on anatomy, sexual health education or biology. Learning about diversity will create an understanding and respect for the diversity that's out there ♡
What is the vulva?
The vulva consists of the external part of the genitalia. It includes the mons pubis, the inner labia and outer labia, the clitoris and the clitoral hood, the urethral opening, the vaginal opening, the hymen, Skene’s glands, Bartholin’s glands and pubic hair. The entrance of the vagina is part of the vulva, but the vagina itself is not. The vagina is one part of the internal structure of the genitalia; it’s the passage between the vulva and the uterus, although it’s important to keep in mind that not all of us with a vulva and vagina have a uterus. This may be the case, for example, when an individual is born with an intersex variation. Another example occurs in those who have undergone gender affirmation surgery. You can find more information about this on the Useful Websites page.
A vulva as seen from below. Find more anatomy images in my book “A Celebration of Vulva Diversity” (click to view).
Mons pubis
The mons pubis (also called mons Venus or pubic mound) is the hairy area above the pubic bone (or the hill at the top of the vulva) and covering the pubic bone (you can feel the bone underneath the soft tissue if you press on it). It consists largely of fatty tissue, and its skin contains hair, sweat glands and many nerve endings, which makes it a sensitive area. The mons pubis divides into the outer labia on either side; the point at which the labia divide is called the pudendal cleft. The fatty tissue of the mons pubis protects the pubic bone, like a soft cushion. The size of the mons pubis varies according to hormone levels and body fat, and there are many possible variations in shape and size; the mons pubis can be skinny or chubby, round or flat. If you gain or lose weight, you may notice that the shape of your mons pubis changes as well. As the fatty tissue of the mons pubis is sensitive to the hormone oestrogen, the shape of the mons pubis may change (and become more prominent) with the onset of puberty. After menopause, due to the decrease in oestrogen, the mons pubis may change in shape again.
A vulva as seen from the front. Find more anatomy images in my book “A Celebration of Vulva Diversity” (click to view).
Pubic hair
Pubic hair is hair that grows around your genitals. With the onset of puberty, hair starts growing on the mons pubis. In the beginning, the pubic hair is soft and thin, but during puberty the hair typically grows thicker, darker and more dense. Over time, pubic hair will also begin growing on the outer labia, between the buttocks and around the anus, towards the stomach and onto the groin area.
As pubic hair is sensitive to hormones, you may find that during your life the amount of pubic hair, its colour, texture and shape may change due to changes in hormone levels. After menopause, due to the decrease in oestrogen, pubic hair often becomes whiter, thinner and more sparse.
Pubic hair has many benefits: it protects the vulva and vagina from dirt, viruses and bacteria, it helps to control the moisture of the skin and decreases the chances of yeast infection and skin irritation. Yay for pubic hair!
Some additional notes for anyone who is insecure about their pubic hair growth
* There are many different possible pubic hair variations. It can be curly or straight, dense or sparse hair, blonde or black or ginger or white, with bald spots, white spots or even entirely bald – these are all common variations
* It's absolutely common to have pubic hair growing between your bum cheeks, on your groin or up to your navel. Body hair doesn't have anything to do with gender and it's perfectly fine to keep your body hair if that makes you happy 👏
* "Excessive" body hair is not a thing, it's an idea that's been created to make people feel bad about their bodies. As there are millions of variations, some of us will have lots of body hair and others will have (almost) no body hair – these variations are all valid and worthy of love.
There’s as much variety in pubic hair growth as there is in human bodies! ♡
Outer labia
The outer labia (or outer lips) start at the mons pubis, part at the pudendal cleft and either cover or ‘hug’ the inner labia. They usually cover the vulvar vestibule (the area surrounding the vaginal opening and urethral opening) and they meet at the perineum. The outer labia consist mainly of fatty tissue, which protects the delicate tissue underneath against impacts. They also contain a thin layer of muscle and erectile tissue, along with many sweat glands, sebaceous glands, nerve endings, hair follicles and many small blood vessels. Because they are so vascular, the outer labia will swell and become more sensitive during arousal. The outer labia change in appearance during a lifespan; during puberty they may change in colour and often become a darker hue, and hair starts to grow on the outer part of the labia. After menopause, lower hormone levels may change the shape of the outer labia again, causing them to become thinner.
A vulva as seen from below. Find more anatomy images in my book “A Celebration of Vulva Diversity” (click to view).
Inner labia
The inner labia (singular: labium) ) are the two hairless folds of skin in between the outer labia. The inner labia are often called ‘labia minora’ (small lips), but this name doesn’t really fit as the inner labia are often longer and more prominent than the outer labia. The inner labia extend from the frenulum of the clitoral glans towards the back of the vulva, and join there in a fold of skin called the fourchette.
The inner labia contain many nerve endings, blood vessels and erectile tissue, as well as sweat glands, scent glands and sebaceous glands. The sebaceous glands secrete mucus that protects the inner part of the vulva from dryness and chafing.
The inner labia vary greatly in size, from barely visible to up to several centimetres long (10 cm / 4 in isn’t uncommon), and they are often asymmetrical. The colour of the inner labia can range from pink to reddish to purplish to brownish or black. Such diversity is common and part of the natural variety in colours.
A vulva as seen from below. Find more anatomy images in my book “A Celebration of Vulva Diversity” (click to view).
Like the outer labia, the inner labia may change quite a lot during a lifespan. With the onset of puberty, due to changes in hormone levels, they often become larger and they may darken in colour. The shape and colour of the inner labia continue to change during your lifespan, due to changes in hormone levels. Pregnancy often changes the shape and colour of the inner labia, causing them to become darker and bigger. After menopause the inner labia may change in shape again, causing them to become smaller and thinner.
What is their function?
The function of the inner labia is to protect your vulvar vestibule and vagina from irritation and friction, and from bacteria and dirt. As the inner labia contain many nerve endings, blood vessels and erectile tissue, they can serve a very important function during sexual activities. When you're aroused, more blood flows to the inner labia: they become more sensitive and swell up, making the labia function as a ‘cushion’, which makes a lot of sex acts more comfortable.
Finally: inner labia are often asymmetrical. Instead of thinking of them as identical twins, you can see them as siblings! :)
Clitoris
The clitoris is a wonderful part of human anatomy, devoted purely to sexual pleasure! It is an erectile organ and has the same embryonic origin as the penis. The two organs are thus very similar in shape and function. They both fill up with blood upon sexual arousal and become erect – so yes indeed, if you have a clitoris, you can have erections too!
The clitoris consists of a glans, a body, two pillars (or crura) and bulbs. Only the glans and part of the body are external, the rest of the organ is buried under the vulva and sits around the urethra and the vagina. The glans varies greatly in size, from barely visible to up to several centimetres long; it isn’t always visible, sometimes only showing itself during arousal (when getting erect).
The clitoral hood is a fold of skin that covers (or ‘hugs’) the clitoral glans. It varies in size from person to person; it can be small or large, and it protects the shaft and (in some cases) the sensitive clitoral glans from chafing and dryness.
The glans and the external part of the clitoral body are often covered by the clitoral hood. They are located at the pudendal cleft of the vulva. Two clitoral bulbs (or vestibular bulbs) are connected to the clitoral body via a complex network of very small blood vessels and are located underneath the crura. These bulbs surround the vaginal canal and are made of spongy erectile tissue, which increases substantially in volume upon arousal.
The clitoris contains many sensory nerves, especially at the surface of the glans and in the body. Some of the nerve endings are like those found in other areas of the body (which detect pressure, vibration, temperature and pain) but some are found only in the clitoris and are specific to sexual arousal. The clitoris and the penis have a similar number of these nerve endings but as the clitoral glans is smaller, they are more dense, which may make the clitoris more sensitive.
Vaginal opening
The vaginal opening is also part of the vulva. It’s the entrance of the vagina, and it is located in between the urethra and the perineum.
Urethral opening
The urethral opening is a small opening located in between the vaginal opening and the clitoral glans. This is where you urinate from.
Perineum
The perineum is a complex structure that lines the pelvic floor and is important for continence and pleasure; it includes several muscles and tendons that are attached to the tailbone and pelvis. Its centre is under the skin that lies between the vulva and the anus. It’s a sensitive area, as the muscles underneath the skin contain many sensory nerves and blood vessels.
A clitoris in erect state. It is fully swollen, with full and round vestibular bulbs. Find more anatomy images in my book “A Celebration of Vulva Diversity” (click to view).
A clitoris in non-erect state. The vestibular bulbs aren’t swollen and are resting peacefully. Find more anatomy images in my book “A Celebration of Vulva Diversity” (click to view).
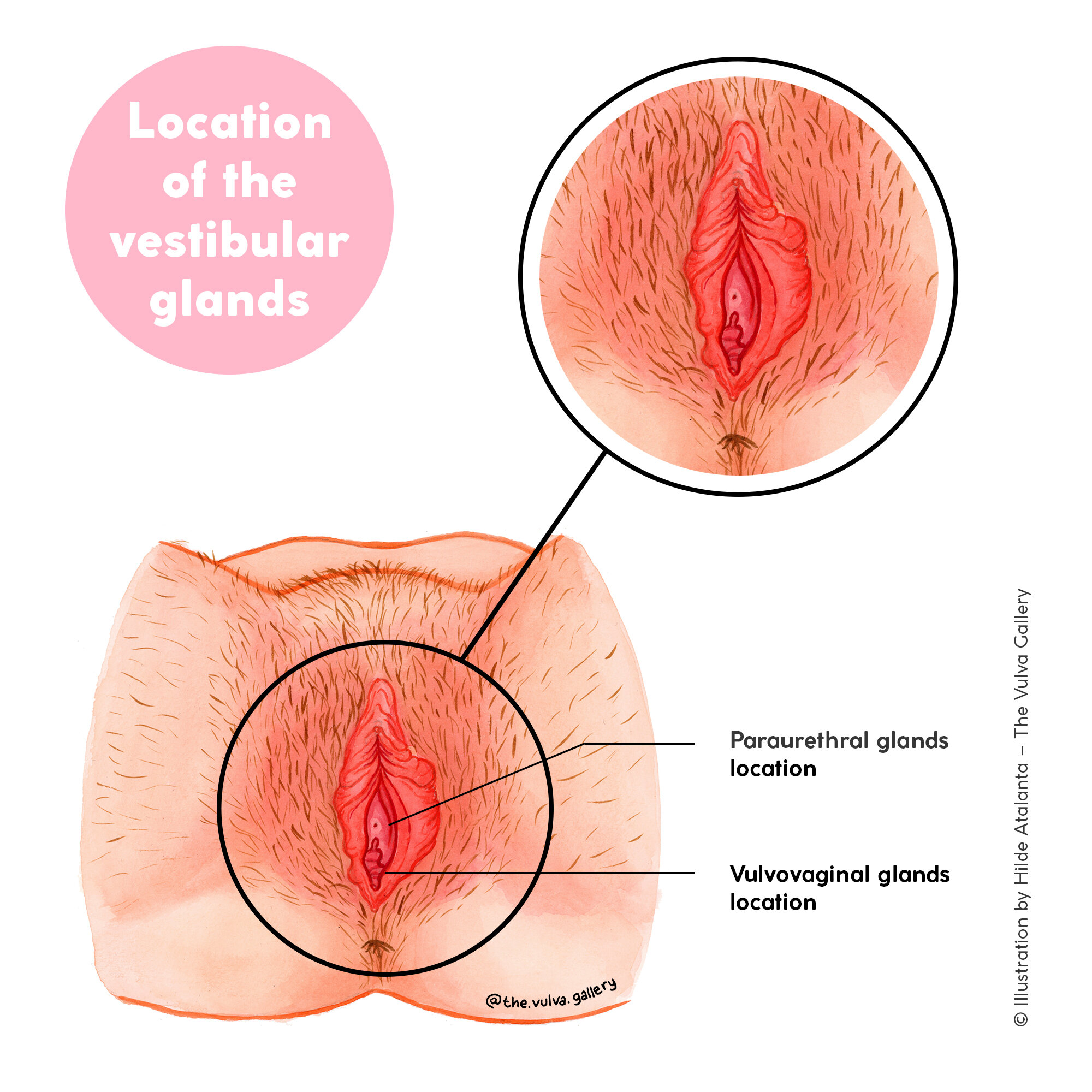
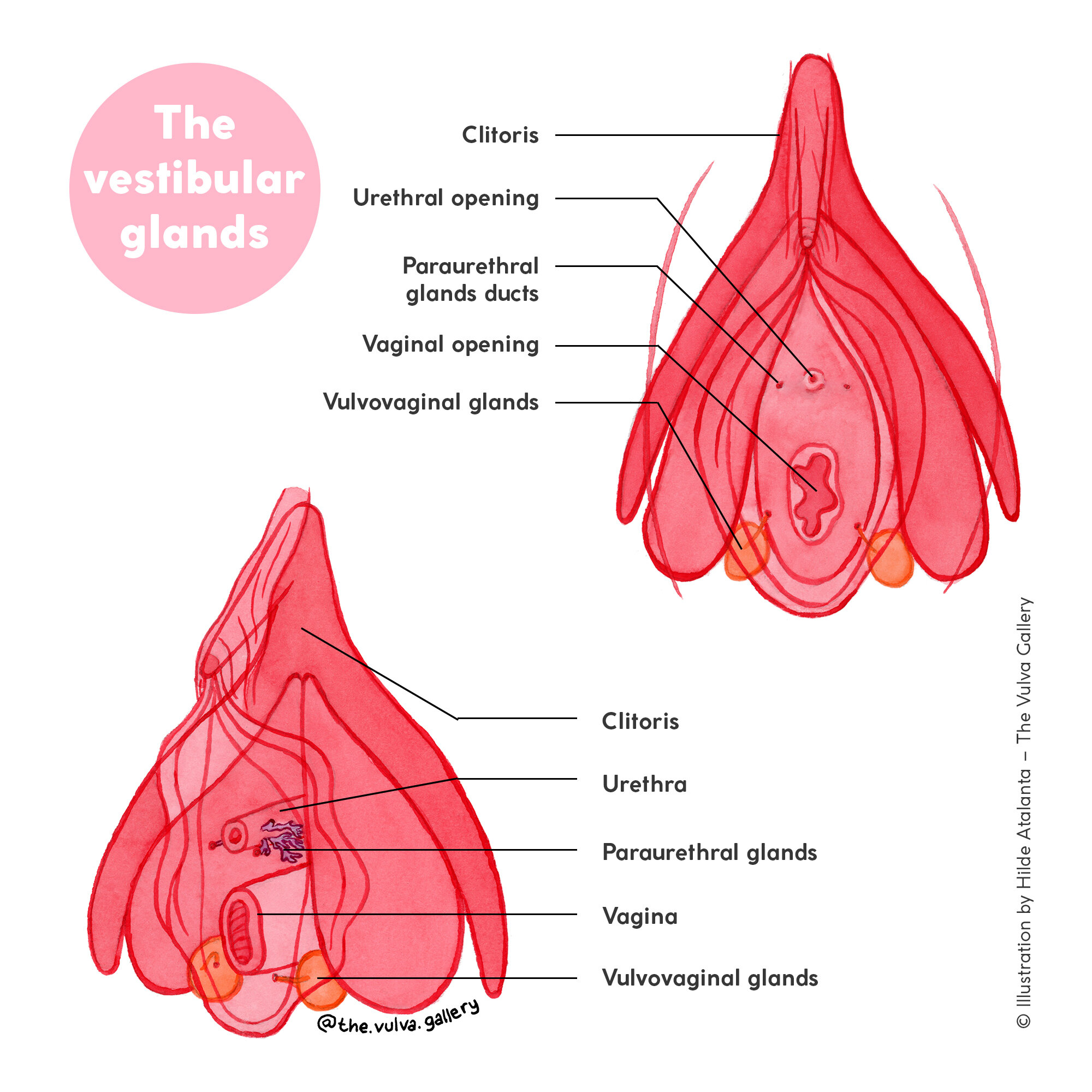

Paraurethral glands and Vulvovaginal glands
The vulva contains two pairs of glands: Paraurethral glands and Vulvovaginal glands. Both glands produce a transparent fluid with a moisturising effect.
The paraurethral glands are located at both sides of the urethra (you can see two tiny holes at each side of the urethral opening). They produce fluid that helps lubricate the urethral opening (and possibly protect it from infections), and they also secrete fluid during orgasm. The glands have similar microanatomical structures to the prostate gland (such as secretory cells) and they also produce prostate specific antigen (PSA). The fluid coming from the paraurethral glands is similar to the fluid produced in the prostate, but the paraurethral glands aren’t exclusively ‘prostate glands’.
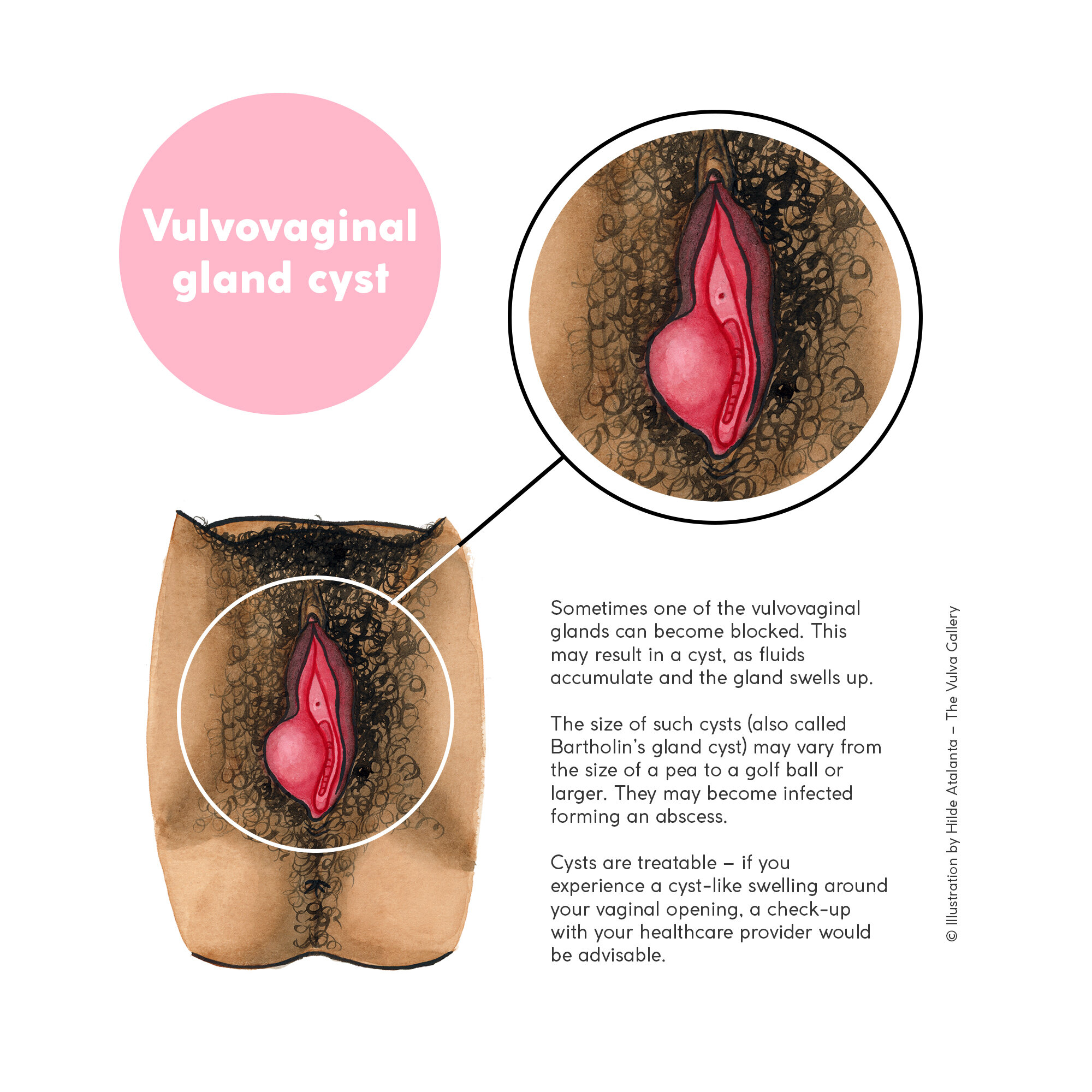
The vulvovaginal glands are two small glands located below the vaginal opening (when lying down). If you look with a mirror you can see two tiny holes, one on each side of the vaginal opening (at 5 and 7 o’clock). The vulvovaginal glands play an important role in lubricating the area around the vaginal opening, thereby making sure that the delicate tissue around the vaginal opening is protected and contact feels smooth. The vagina itself however doesn’t get lubricated by the glands.
“So… how does my vagina get lubricated then?” Well, that’s an interesting question! Lubrication of the vagina happens through the mucous membranes that cover the vaginal walls (another example of mucous membranes is the inside of your mouth). As the vaginal lining has no glands, the vagina relies on other methods of lubrication. When you get aroused, blood flow increases, and due to increased pressure in the blood vessels, blood plasma (the liquid part of your blood) is pressed through the vaginal walls. This is considered to be the major source of vaginal lubrication. Near ovulation, cervical fluid provides additional lubrication (which is transparent and very elastic fluid). Yay for the wonders of our vulvas and vaginas!
Hymen
The hymen is a small, flexible tissue that forms a ridge around the vaginal opening. The hymen consists of thin folds of mucous tissue. The colour is very light pink (almost transparent) and usually it is elastic and stretchy. It varies in size, colour and shape, and can even be absent – independent of sexual activity.
There are several other possible variations of hymen shapes, for example, a microperforate hymen, in which there’s a very tiny hole; a septate hymen in which the membrane has a band of extra tissue in the middle, creating two openings instead of one; or a cribriform hymen in which the membrane has many tiny holes.
Sometimes the hymen may cause problems, for example when it is imperforate (covering the whole vaginal opening), when it’s microperforate (in which there’s a very tiny hole), when it’s septate (in which there is an extra band(s) of tissue in the middle), or when it’s cribriform (in which there are many tiny holes). A gynaecologist can open the hymen to release menstrual blood, and enable you to use tampons or have insertive sex.
The shape of the hymen may change naturally due to hormones, by masturbation or by using tampons. Some of the changes may already happen during childhood and puberty. For the reasons mentioned it is impossible to know whether someone has had sexual intercourse by looking at their hymen – even the most experienced doctors cannot assess this.
Vulvas as seen from below. Find more anatomy images in my book “A Celebration of Vulva Diversity” (click to view).
As the hymen is a very flexible membrane, it usually doesn’t ‘tear’ during the first time of having sexual intercourse. However if you’re tense, minor ruptures can happen and these may sting or bleed a little (they usually heal within a day) – but this has nothing to do with how often you’ve had sex. Bleeding during the first time may happen due to small tears in the skin of the fourchette, if an individual is tense and/or not aroused and lubricated enough or if the person they have intercourse with enters the vagina too fast. Pain or bleeding during sexual intercourse is not something you ‘have to go through’.
The medical procedure to ‘fix’ the hymen after it’s ‘broken’ is therefore an unnecessary procedure, merely performed for cultural or religious purposes – it will not turn a person back into being a ‘virgin’.
Side note: The term ‘virgin’ is commonly used to describe a person who hasn’t had vaginal intercourse yet. I prefer to avoid using it as it comes from a heteronormative belief in which ‘sex’ means sexual intercourse between a man and a woman, and that losing your ‘virginity’ is a negative thing; and that being a ‘virgin’ is highly valued and linked to a woman's desirability and worth. I feel it’s very important to emphasise that there are many different ways of having sex (between people of all kinds of genders) that don’t include vaginal intercourse. It’s up to you and you alone to figure out what your sexual preferences and needs are. When sexual activities, in whichever form, are enjoyed between consenting adults, it’s a good thing and nothing to be shamed for. No matter the number of sexual encounters you have had in your life, whether it’s zero or thousands, you are always of worth.